Heavy menstrual bleeding or menorrhagia is defined as menstrual bleeding with a loss of blood of 80 ml or more per cycle.
There are many ways to measure the loss of blood during menstruation. The methods are:
Subjective estimate (number of pads, clots, breakthrough bleeding)
Semi-subjective estimate
Anemia
Counting the number of days of menstruation
Alkaline hematine method
Pictorial blood loss chart
Weighing sanitary products
However, today we believe that such estimates are unnecessary. It has been proven that only half of patients complaining of heavy menstrual bleeding and actually do have such cycles confirmed by objective measurements, test normal when put to blood screenings. For this reason, we consider that testing and treatment of heavy menstrual bleeding are doctors’ response to patients concerns and need to be undertaken in these cases.
Half of heavy menstrual bleedings compose of heavy bleeding caused by organic changes to the organism such as myoma, endometriosis, polyps, etc. The other half consists of heavy bleeding with no proven pathology, the so-called dysfunctional uterine bleeding (DUB). According to recommendations of the European Society for Human Reproduction and Embryology, DUB refers to excessive uterine bleeding which does not occur due to demonstrable organic cause.
We usually estimate that between 15 and 20 percent of all women suffer from heavy menstrual bleeding. 67 percent of those women are anemic and heavy bleeding causes two thirds of all hysterectomies (surgical removal of the uterus). It has been estimated that around 50.000 women in Croatia suffer from heavy menstrual bleeding thus making this diagnosis the most common one the gynecologists tackle with on a daily basis.
Dysfunctional uterine bleeding (DUB) can be ovulatory and anovulatory. There are three most important patterns in anovulatory DUB – it occurs during puberty, in perimenopause or is caused by polycystic ovaries. Ovulatory DUB is considered to be heavy menstrual bleeding with no demonstrable organic cause and is also known as idiopathic or unexplained heavy bleeding.
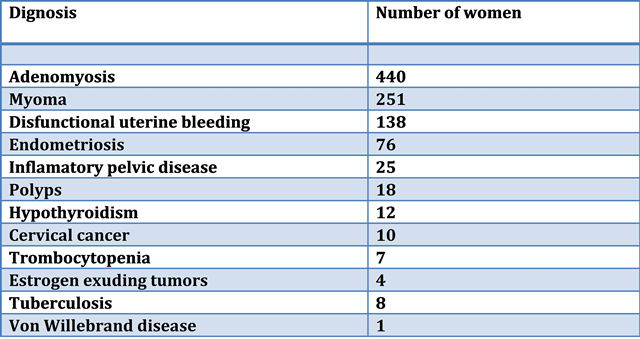
Organic causes of heavy bleeding are numerous. The following table shows a list of heavy bleeding causes in 1.000 consecutive patients in a single clinic.
The table shows that the most common cause of heavy menstrual bleeding recorded in gynecology clinics is adenomyosis. Around 2-3 percent of all women suffer from adenomyosis. In half of those cases the symptom is heavy menstrual bleeding and it is diagnosed using an ultrasound showing increased uterus with asymmetric thickening of the frontal and posterior wall as well as small cysts the size between 1 and 6 mm inside the uterine lining.
All causes of heavy bleeding listed here have some things in common: they are diagnosed in the same way and they can be treated using the same medication.
Dysfunctional uterine bleeding (DUB) can be ovulatory and anovulatory. In a regular menstrual cycle there is a perfect balance of hormones which bring about the final result of menstruation – menstrual bleeding. In cases of anovulatory dysfunctional bleeding the disturbance is in the hormone levels. That is why anovulation occurs (the egg does not leave the ovary during ovulation) and the endometrium is excessively stimulated by estrogen (female hormone mostly exerted prior to ovulation). For this reason breakthrough bleeding occurs.
It is considered that in cases of ovulatory dysfunctional bleeding the problem is not created by hormones, but by increased production of prostaglandin in the endometrium. Patient complaining of heavy bleeding will be taken a case history and in doing so the following questions will have to be answered:
Is there a possibility that the patient is pregnant? Pregnancy is the most common cause of bleeding in young and healthy women.
How many pads/tampons does the patient use, are there any blood clots observed, etc?
How old is the patient? Is she overweight? Has she given birth already? Has she been diagnosed with diabetes, etc?
Some bleeding may be caused by sexually transmitted disease, i.e. by infection of the endometrium caused by STDs, therefore cervical swabs may have to be done.
Does the patient use contraception? If yes, what kind? Intrauterine device increases bleeding.
A number of medication may cause heavy bleeding, including contraception pills. Does the patient have a breast discharge? A large number of systemic diseases of heart, kidneys, liver, thyroid may cause heavy bleeding. Does the patient have a history of longer bleeding from cuts?
Following the case history, a clinical check-up will have to be done – a gynecological check-up, Pap smear and complete blood count. Many tests may be done depending on the case history and the clinical check-up, but they will be done on an exceptional basis.
Laboratory investigations
Cervical swabs, coagulation tests, a pregnancy test, thyroid tests, prolactin level, blood sugar level, hormonal status, liver probes.
Transvaginal ultrasound – the ultrasound needs to be done in case of doubt whether curettage is needed or not. In premenopausal women, endometrial thickness over 10-12 mm is the cut off that should prompt further evaluation.
Endometrial study
Dilatation and Curettage (D&C)
Endometrium biopsy
Hysteroscopy
Endometrial sample for analysis may be obtained by curettage, biopsy or hysteroscopy. Meta analysis of 39 studies from the year 2000 has shown that endometrial biopsy using Pipelle suction curette is better than dilatation, curettage or hysteroscopy in attempts to diagnose endometrial cancer. Indications for these tests are found in women over 40 or younger women resistant to therapy, women with increased endometrial cancer risk (women who have not given birth, overweight women, women with family history of endometrial or bowel cancer, women taking pure estrogen for PCOS or women on tamoxifen).
Treatment
Hormonal treatment of heavy menstrual bleeding is most common in Croatia especially using gestagens such as Duphaston and Provera, levonorgestrel releasing intrauterine system (Mirena), oral contraceptive pills and a hormone supplement therapy.
Oral contraceptives provide an acceptable decrease in blood loss for 50-60%, while levonorgestrel releasing intrauterine systems reduce blood loss for more than 90% proving both therapies prominent in treating heavy bleeding when it is properly indicated.
Besides being efficient contraception and reducing menstrual blood loss, oral contraceptives also reduce menstrual pain, decrease chances of endometrial and ovarian cancer later on as well as protect fertility by reducing the risk of inflammatory pelvic disease, myomas and endometriosis.
Oral contraceptives are used in treating anovulatory dysfunctional bleeding and the treatment usually looks like this: in acute bleeding, 2-3 pills of contraceptive are administered alongside 35 or more mcg of estradiol over the period of 7 days. The dosage may be gradually lowered in order to imitate the usual cycle duration, but this causes heavier bleeding due to longer estrogen stimulation. Therefore, a 7-day treatment is advised.
When using Mirena, the percentage of blood loss reduction is extraordinary after only 3 months of using and remains such even after one year of use. Mirena has proven to be an exceptionally useful medication for women who do not want to undergo hysterectomy.
There are many women in our clinics today who are under increased risk of developing polyposis and endometrial cancer because of tamoxifen therapy. Mirena is a good choice for them. It has also proven useful in some women having myomas, endometriosis or suffering from heavy bleeding for other reasons.